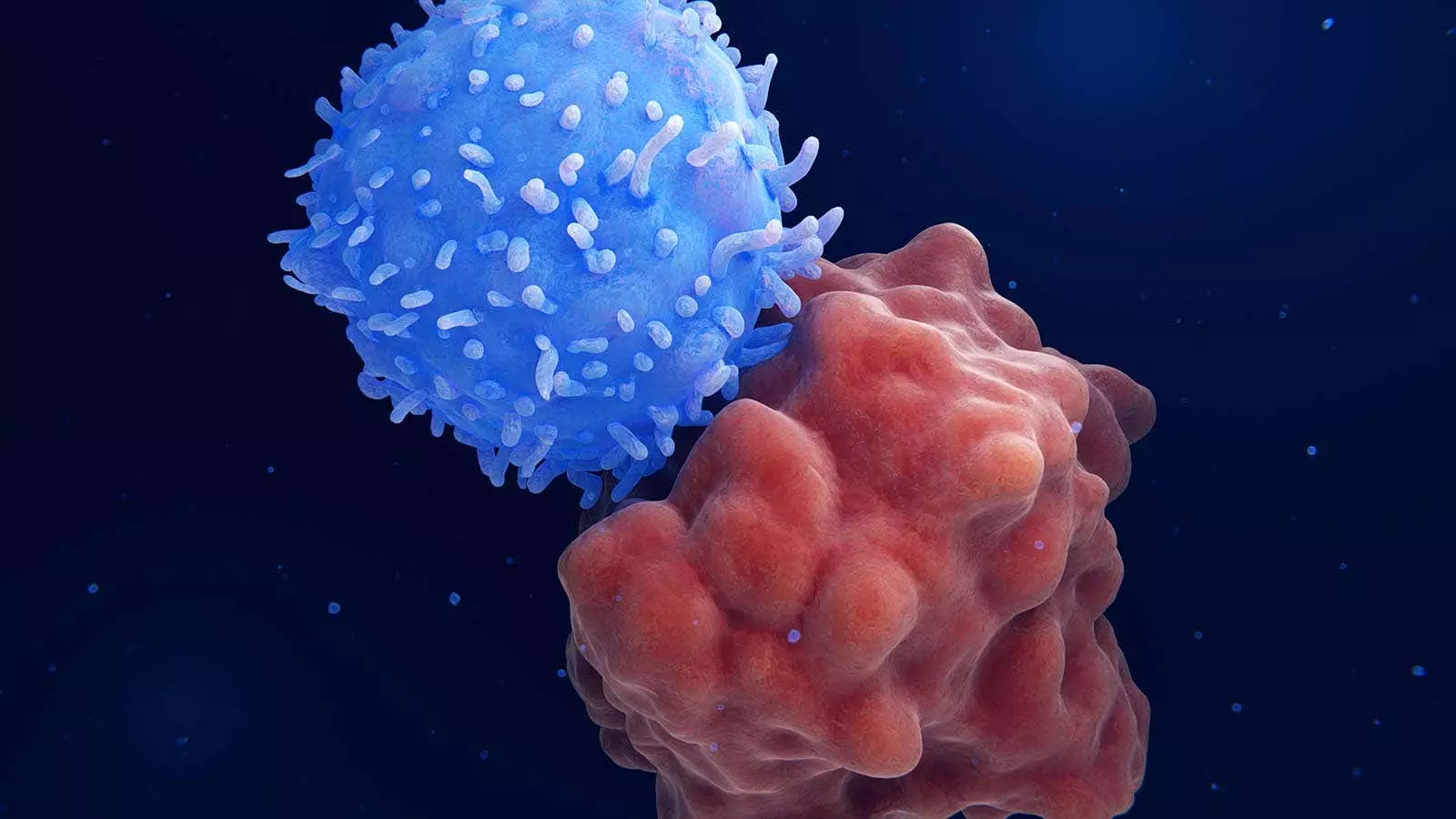
A novel strategy utilizing sequential CD7 chimeric antigen receptor (CAR) T-cell therapy followed by haploidentical hematopoietic stem-cell transplantation (HSCT) has shown promising results for patients with relapsed or refractory hematologic cancers. The approach, proposed by researchers from Zhejiang University School of Medicine in China, involves administering CD7 CAR T-cell therapy to achieve complete remission, followed by haploidentical HSCT without graft-versus-host disease (GVHD) prophylaxis. Out of the 10 patients in the case series, all achieved complete remission post CAR T-cell therapy, with 90% exhibiting minimal residual disease (MRD)-negative incomplete hematologic recovery. The subsequent haploidentical HSCT led to a favorable estimated 1-year overall survival rate of 68%.
The results of this study, though preliminary, have sparked interest in further exploring the “all-in-one” approach in larger cohorts of patients. The insights gained from this innovative strategy have paved the way for considering its application in different clinical scenarios. For instance, the approach is being evaluated as a potential first-line treatment for newly diagnosed CD7-positive acute myeloid leukemia (AML) patients who are not eligible for intensive induction therapy. Moreover, the concept of dual CAR T-cell constructs targeting both CD7 and another antigen for CD7-negative leukemia holds the promise of revolutionizing the treatment landscape for diseases with a grim prognosis.
The rationale for employing this comprehensive strategy stems from the unique expression of CD7 in a substantial proportion of AML cases. By utilizing CAR T-cell therapy as a bridge to allogeneic HSCT, researchers aim to achieve sustained tumor elimination and reduce the risk of cancer relapse. However, the conventional myeloablation and GVHD prophylaxis agents pose challenges by potentially compromising the antitumor effects of CAR T cells. Additionally, patients ineligible for allogeneic HSCT due to underlying health conditions present a significant treatment gap that this innovative approach seeks to address.
Patient Characteristics and Treatment Outcomes
The patient cohort involved in the study comprised ten individuals with relapsed or refractory CD7-positive leukemia or lymphoma. These patients, aged around 56.5 years on average, had undergone extensive prior treatments with a median of 9.5 therapy courses. The remarkable response to the sequential therapy was evident in the complete remission following CAR T-cell therapy in all patients. Notably, the transient cytokine release syndrome (CRS) and manageable cases of GVHD demonstrated the feasibility and safety profile of the approach. Despite two fatalities attributed to severe infections, the overall outcomes were promising, warranting further investigation into the long-term efficacy and safety of this strategic approach.
The integration of sequential CD7 CAR T-cell therapy and haploidentical HSCT represents a promising avenue for patients with challenging hematologic cancers. The success achieved in achieving complete remission and the favorable survival rates underscore the potential of this approach to reshape the treatment landscape. Continuous research and refinement of this strategy hold the key to unlocking new dimensions in managing hematologic malignancies, offering hope for patients with otherwise limited therapeutic options.
Leave a Reply