The recent Medicaid rules aimed at implementing minimum nursing home staffing requirements and increasing pay for home care workers have sparked displeasure among House Republicans. Representative Brett Guthrie expressed concerns that while frontline caregivers and clinical care providers deserve better compensation, the proposed approach might not be effective. With over 500 nursing home closures and 150,000 fewer long-term care workers since 2020, the impact of these rules on the healthcare system is a point of contention.
The requirement for nursing homes to have a registered nurse on staff 24/7 and provide 3.5 hours of personalized care per resident per day has raised issues. Representative Cathy McMorris Rodgers highlighted that these staffing mandates could be unattainable, leading to the closure of nursing homes or reductions in services for seniors. Additionally, the 80/20 policy for home care agencies, mandating direct payment to workers, poses challenges in service provision.
House Republicans have swiftly introduced bills to counter the new regulations. H.R. 7513 seeks to halt the implementation of nursing home staffing rules, while H.R. 8114 aims to block the 80/20 pay rule for home care workers. The resistance from Republican lawmakers indicates a significant divide on the feasibility and impact of the proposed changes on the Medicaid system.
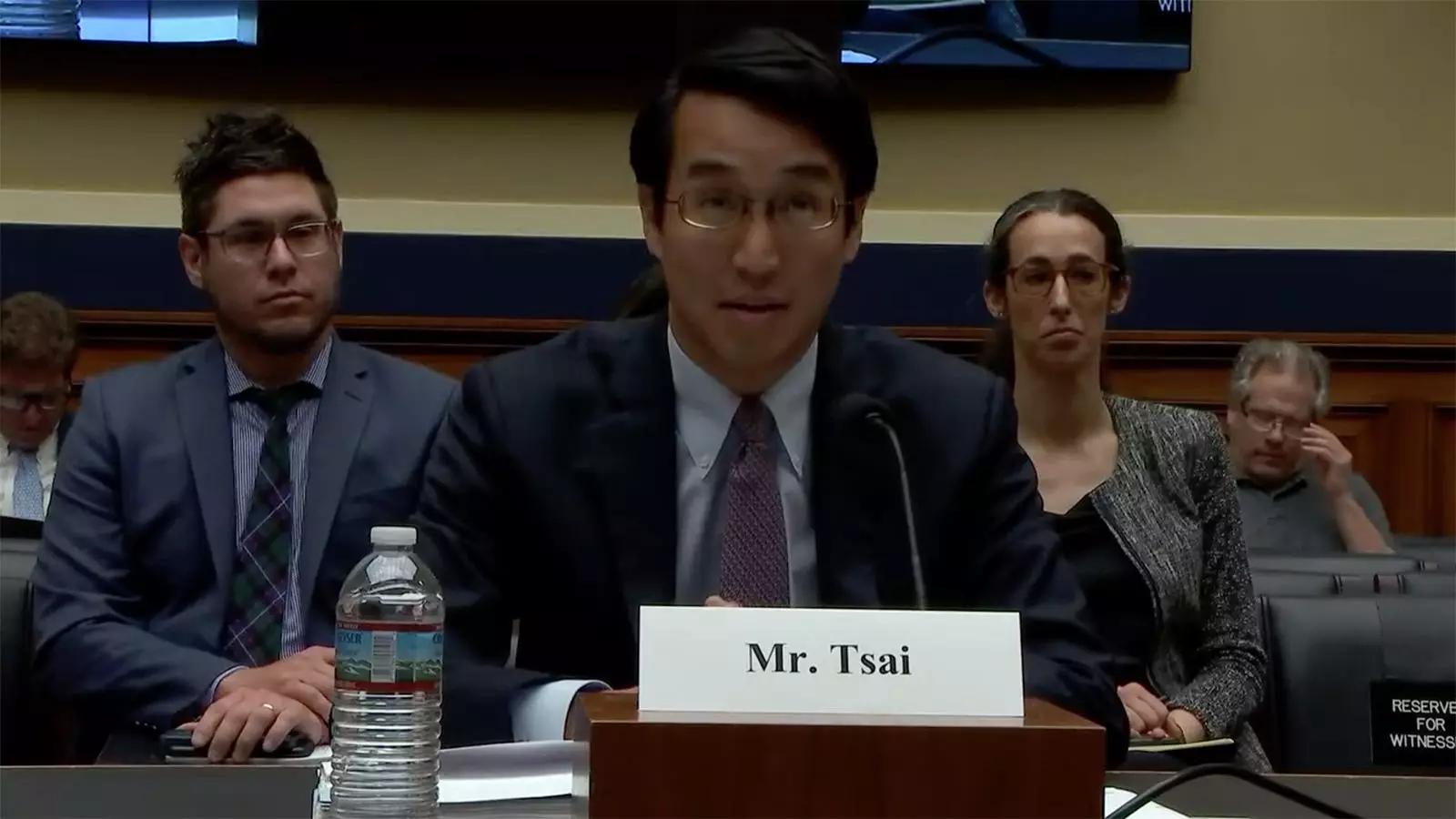
Despite the Republican backlash, Daniel Tsai from the Centers for Medicare & Medicaid Services defended the nursing home rules. He emphasized the need to balance workforce challenges and quality care, asserting that the regulations offer standards with provisions for implementation timelines and exceptions based on workforce shortages. Committee Democrats commended the administration’s rulemaking as a step towards enhancing nursing home quality and caregiver wages.
The discussion at the hearing extended to other Medicaid-related bills proposed by committee members. Representative Rogers highlighted bipartisan efforts with Representative Pallone to address states’ waitlists for home and community-based services. Proposals like making the “Money Follows the Person” program permanent and advocating for increased flexibility in service provision showcased a commitment to enhancing Medicaid services.
Legislators like Representative Dingell focused on initiatives like the “Money Follows the Person” program that facilitate smooth transitions from nursing home care to community-based services. The bipartisan backing for these programs underscores their efficacy in improving patient outcomes, reducing costs, and promoting care continuity.
Representative Schakowsky raised concerns about the Medicaid Estate Recovery Program, highlighting its impact on families of deceased recipients. The program’s implications on low-income households and the punitive nature of recovering costs post-bereavement were central to her criticism. The need for a more humane and effective approach in addressing these financial burdens became a point of contention in the discussion.
Overall, the debates surrounding the Medicaid regulations underscore the complexities of healthcare policy implementation and the divergent perspectives on balancing care quality, workforce considerations, and financial sustainability within the Medicaid system. As policymakers navigate these challenges, a collaborative and evidence-based approach will be crucial in shaping the future of Medicaid services for vulnerable populations.
Leave a Reply